My Journey – a diary
You have WHAT?
My reaction exactly.
June 2024
This story begins in early summer. During my annual exam at a local medical clinic, I showed the physician’s assistant a lump in the webbing between my thumb and index finger on my left hand. I’d noticed it for a few weeks and thought maybe it was a bug bite. The PA felt the lump, then pronounced it to be some sort of cyst that would cost $1,000+ to remove surgically.
I promptly forgot about it.
July 2024
While at my annual dermatology visit, I stuck out my hand and showed the doctor my lump. Likewise, she felt it.
“Oh, that’s Dupuytren’s contracture,” she said.
“That’s WHAT?” I replied.
“Dupuytren’s,” she repeated.
“Could you please write that down for me?”
“Sure.” The doctor tore off a piece of paper and scribbled Dupuytren’s contracture in black ink. I stared at the words, then stuck the paper in my purse.
There it remained until I began to notice the lump more and more. Grudgingly, I pulled out the paper and Googled the name. That’s when I began to learn not only how to say and spell Dupuytren, but how I looked to be headed for a challenging health issue at age 65. On Facebook, I joined several Dupuytren groups.
What is Dupuytren’s disease?
According to Johns Hopkins Medicine, “Dupuytren’s contracture (also called Dupuytren’s disease) is an abnormal thickening of the skin in the palm of your hand at the base of your fingers. This thickened area may develop into a hard lump or thick band. Over time, it can cause one or more fingers to curl (contract), or pull sideways or in toward your palm. The ring and little fingers are most commonly affected. In many cases, it affects both hands." Feet may also be affected.
According to what I’ve read, the disease is believed to be hereditary. It may also be linked to smoking, alcoholism, diabetes, nutritional deficiencies or medicines used to treat seizures.
I fit none of those profiles.
By the way, the disease is named for Baron Guillaume Dupuytren, a French surgeon who described and developed the first surgical procedures to alleviate what became known as "Dupuytren's contracture."
September 2024
After asking around, I made an appointment with an orthopedic surgeon in the Hill Country. At his clinic, a technician took three x-rays of my hand in different positions. Later, the doctor stepped into the exam room to look at my hand.
“Yep, you’ve got Dupuytren’s,” he said matter-of-factly.
In a nutshell, he said the only solution – because there is no cure – was to remove the nodules via surgery. He shook his head at other medical alternatives, such as shots or radiation. Too expensive, he said.
“All we can do is monitor your hand,” he said. “Come back in six months, and we’ll take another look.”
I got back on Facebook and started asking questions in my Dupuytren groups. I also cancelled my follow-up with the orthopedic surgeon.
October 2024
One evening, James, my husband, and I took a bike ride in the neighborhood. Fifteen or so minutes later, I noticed my left hand begin to ache. So I lessened my grip on the handlebar and then completely let go. I must have “awakened the monster,” as Dupuytren patients say, because my nodules began to grow and increase. My hand aches and tingles sometimes. It's not pleasant.
Thanks to this odd condition, I've become more aware of others who suffer with it. While at a recent Texas Master Naturalist conference, a nice gentleman and I attended several of the same sessions. I'd noticed that the fingers on one of his hands were drawn up and contracted. Finally, I got up my nerve, leaned over to him, and stuck out my left hand.
"Do you have what I have?" I asked.
He nodded. "Yes, my father had it," he said. Thankfully, the gentleman said he has no associated pain with his Dupuytren's contracture.
In the meantime, I reached out to Debra, a Texan in one of my Facebook groups, and asked if she could recommend a radiation specialist. From what I’d read, low radiation therapy seemed to be my best option for relief. She said yes and reached out to her oncologist. He got right back to her!
On a Saturday morning, October 12, I emailed Dr. Shalin Shah (pronounced “shaw”) with MD Anderson Cancer Center in Sugarland, Texas, and requested an online consultation. By that evening, he emailed me back!
October 31, 2024 – Consultation with Dr. Shah
Via Zoom, Dr. Shah met with me and shared a slideshow to help explain this disease. He ultimately recommended that I proceed with low radiation therapy on my left hand. Here are some of Dr. Shah’s thoughts and observations during our visit, which I recorded (with his permission):
THANK YOU, DR. SHAH! For more information, Dr. Shah has two videos on his YouTube channel.
I am moving forward to seek radiation treatment from a radiation oncologist at the Mays Cancer Center/MD Anderson Cancer Center in San Antonio. I will update this page as I go along.
First step: Schedule a CT simulation that will be used to map out the area of treatment on my left hand. After that, five days radiation followed by 10 or so weeks off. Dr. Ha will check my hand for any changes, then I'll return for five more days of radiation.
"Have you treated anyone with Dupuytren's before?" I asked.
Dr. Ha shook his head. "No."
"Oh, then I'll be your first," I exclaimed.
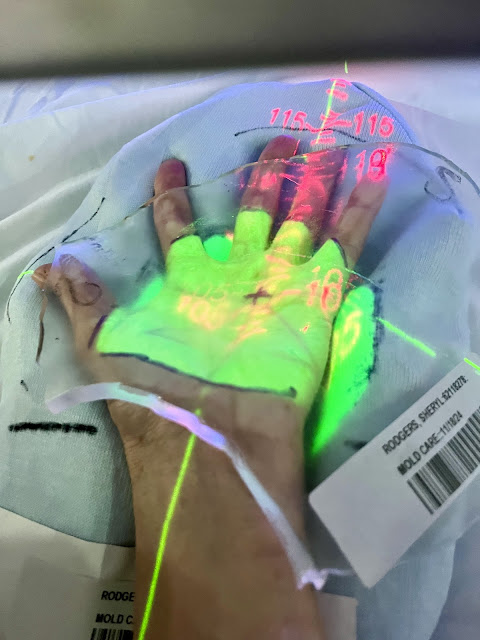
We arrived at Mays Cancer Center in San Antonio by 8:45 a.m. Right before 9, Louis – one of two CT technicians – escorted me to the imaging room. I was happy when I saw Dr. John Yassa appear. Right away, Louis had me lay down on a table. It took a little bit of time before I found just the right position.
"Oh, this is how I sleep," I noted after finally getting adjusted on my left side. A flat blue block propped my head up. Above me, my left hand stretched out awkwardly, palm up on the table. By then, Nickie – the other CT tech – stepped into the room. So did Dr. Chul Ha. That's the moment my eyes welled up, and emotion got the better of me.
All these people are here to take care of me. I am so blessed. A tear leaked from my right eye down to the bridge of my nose. James, my husband, leaned over me. "You ok?"
"I'm just so grateful," I said. A few more tears escaped.
"Oh, I've seen this before," Nickie commented. "We had at least two patients where I was before, and they had good success with radiation." That gave me more encouragement.
"Now I'm going to give you some tattoos," he said.
My first thoughts: Do I get to pick? Will they wash off?….
"Yep. They'll look like little freckles. Like this one." Louis held out one of his hands and pointed to a spot on his palm. The black dot was barely visible.
"Oh, my first tattoos!"
Louis laughed. "See? Something good came out of today."
"My daughter will be so impressed," I quipped.
Moving forward, my CT simulation from today will be used to map out the radiation areas on my hand. My first round of treatments has been scheduled for December 9-13.
Dr. Chul Ha, accompanied by Dr. John Yassa, came into the room briefly with his laptop computer. He conferred with Jeff and Jasmine, the other radiation therapist, as they worked to arrange my hand just right. At one point, they marked my left hand with a purple marker. On the table, I stared sideways at a beautiful framed digital photograph of the sea while the radiation team exchanged numbers back and forth. Overhead piped-in singers crooned lyrics from the '80s.
For the next 10 weeks, I'm going to write a weekly update during this time of "rest" between radiation treatments. Last Friday, I had the last of five consecutive treatments on my left hand at Mays Cancer Center. I've already been asked by a couple of Dupuytren friends how I'm doing (both started their radiation this week).
No redness as yet in my hand. I'm feeling about the same, no fatigue. However, my nodules seem a little harder and more sensitive. If I accidentally bump one, YIKES! My hand aches sometimes but not too bad at all.
My left hand is about the same this week. Some stinging, aching, tightness around the nodules.
January 8, 2025 – Week #4
I can't put my left hand around a glass or mug without discomfort. The nodules are about the same – sometimes tender. Often tight feeling or like bruised. On a pain level, it's 1 or 2 – Thank the Lord for that!
My left hand has been uncomfortable and tight. The nodules seem harder. A week or so ago, I messaged Dr. Shah.
Dr. Shah wrote back: "Yes, this is totally normal and the result of mild swelling after the first course. Dr. Ha will likely examine you prior to your second course to confirm. For now, conservative management with ibuprofen, cold packs can help with the swelling. If you need something stronger, Dr. Ha can prescribe a medrol dose pack."
This morning, I met with Dr. Brian Fricke with the Department of Physical Medicine at the Mays Cancer Center in San Antonio. Once again, I feel like I've landed in really good hands. I officially have my quarterback now! Plus, he's young so I will definitely outlast him. LOL!
 |
| Left hand |
 |
| Right hand |
 |
| How can I be smiling? I've got to! |
 |
| Right hand |
 |
| Left hand |
LEFT HAND: Thickening of the palmar fascia extending to the ulnar aspect of the third finger at the metacarpophalangeal joint, in line with the fourth finger. Additional thickening noted in the first web space. Radial abduction of the left thumb measured at 40 degrees. Metacarpophalangeal contracture of the middle finger of 13 degrees. Other fingers without hyperextension. Full flexion achieved.
RIGHT HAND: Thickening of the palmar fascia in line with the ring finger and extending toward the third finger. No palpable Dupuytren's in the first web space. One nodule proximal to the metacarpophalangeal flexion crease of the index finger. Right fifth finger hyperextends to 20 degrees at the metacarpophalangeal joint. Proximal interphalangeal joint of the fifth finger at 20 degrees of flexion, passively extensible. Index and ring finger proximal interphalangeal joints at 15 degrees of flexion, both passively extensible. Full flexion achieved.
Dr. Drukker told me that he wouldn't have recommended radiation on my left hand unless I was a younger person with more years ahead of me. Why not radiation at my age? I need to ask that follow-up question.
I agreed to discontinue using the Verapamil gel. It seems to make both my hands ache and burn slightly. I will return in three months for more measurements.































Comments
Post a Comment